Elias Vogel
Since the year 2000, the global fight against malaria has made a steady series of advances. Sadly, that downward trend has come to an end. Especially in Sub-Sahara Africa, the disease is again on the rise with a growing number of cases since 2017.
One of public health’s greatest triumphs
Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes. Malaria occurs mostly in poor tropical and subtropical areas of the world. In many of the countries affected by malaria, it is a leading cause of illness and death. In areas with high transmission, the most vulnerable groups are young children, who have not developed immunity to malaria yet, and pregnant women, whose immunity has been decreased by pregnancy. The cost of malaria – to individuals, families, communities, nations – are enormous. People who have malaria usually feel very sick, with a high fever, heavy chills, headache, vomiting, muscle pain and fatigue. Some people who have malaria experience cycles of malaria attacks. An attack usually starts with shivering and chills, followed by a high fever, followed by sweating and a return to normal temperature. Malaria signs and symptoms typically begin within a few weeks after being bitten by an infected mosquito. However, some types of malaria parasites can lie dormant in your body for up to a year. It is a preventable and curable disease. While the disease is uncommon in temperate climates, malaria is still common in tropical and subtropical countries. World health officials are trying to reduce the incidence of malaria. This fight against malaria has been very successful. There has been a decade of steady advances. Vector control is the main way to prevent and reduce malaria transmission. Vector control measures depend on vector species, mosquito biology, cost and acceptability by populations. The main current measures are focused on reduction of the contact between mosquitos and humans, the destruction of larvae by environmental management and the use of larvicides or mosquito larvae predators, and destruction of adult mosquitoes by indoor residual spraying and insecticide-treated bed nets. Besides vector control, there are also personal protection measures against mosquito bites. Because of the nocturnal feeding habits of most Anopheles mosquitos, malaria transmission occurs primarily at night. Protection against mosquito bites include the use of mosquito bed nets, the wearing of clothes that cover most of the body and use of insect repellent on exposed skin. There are also different drugs to prevent malaria. These drugs are often taken by tourists visiting regions where malaria is common. There are different drugs recommended depending on the country that is visited. No antimalaria drug is 100% protective and must be combined with the use of personal protective measure. Once someone is infected with malaria, there are different treatments. Treatment of malaria depends on many factors, including disease severity, the species of malaria parasite causing the infection, and the part of the world in which the infection was acquired. The latter two characteristics help determine the probability that the organism is resistant to certain antimalaria drugs. Additional factors such as age, weight, and pregnancy status may limit the available options for malaria treatmen.
The incidence rate of malaria declined globally between 2010 and 2018, from 71 to 57 cases per 1000 population at risk. Mortality caused by the disease plummeted by nearly 60%. These results are seen as one of public health’s greatest triumphs. But even today, malaria is a threat that is not to be underestimated. Approximately 70% of the world’s malaria burden is concentrated in just 11 countries – 10 in sub-Saharan Africa (Burkina Faso, Cameroon, Democratic Republic of the Congo, Ghana, Mali, Mozambique, Niger, Nigeria, Uganda and United Republic of Tanzania) and India. These high-burden nations are home to an estimated 151 million cases of malaria and 275 000 deaths.
A massive wake-up call
In recent years the process of successfully fighting malaria has stalled, and the number of new malaria cases worldwide could not be significantly reduced. The biggest risk factor for developing malaria is to live in or to visit areas where the disease is common. There are many different varieties of malaria parasites. The variety that causes the most serious complications is most commonly found in African countries south of the Sahara Desert, the Asian subcontinent, New Guinea, the Dominican Republic and Haiti. Scientists around the world are trying to develop an effective vaccine for malaria. As of yet, however, there is still no malaria vaccine approved for human use. The complexity o the malaria parasite makes development of a malaria vaccine a very difficult task. Over 20 vaccine constructs are currently being evaluated in clinical trials or are in advanced preclinical development. Poverty, lack of knowledge, and little or no access to health care are contributing to malaria deaths worldwide. Malaria imposes substantial cost to both individuals and governments. Costs to individuals and their families include purchase of drugs for treating malaria at home, lost days at work, absence from school and expanses for preventive measures. Costs to governments include maintenance, supply and staffing of health facilities, purchase of drugs and supplies and public health interventions against malaria, such as insecticide spraying or distribution of insecticide-treated bed nets. Direct costs have been estimated to be at least 12 billion USD per year. The cost in lost economic growth is many times more than that.
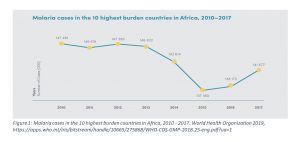
According to the World malaria report 2018, there were globally 219 million cases of the disease in 2017, compared to 217 million the year before. In 2017, all of the 10 highest burden African countries reported increases in malaria cases over the previous year, ranging from an estimated 131 000 more cases in Cameroon to 1.3 million additional cases in Nigeria. Only India marked progress in reducing its disease burden, registering a 24% decrease compared to 2016. In total, among the 10 highest burden African countries, there were 3.5 million more cases in 2017 over the previous year. (Figure 1) These numbers cause great concern among the global community and represent a massive wake-up call. The fight against malaria has not been won yet!
”High burden to high impact”
The numbers show that there needs to be a new approach in combating the disease and even more ambitious goals for the future. The goal of most current national malaria control programs is to reduce the number of malaria-related cases and deaths. To reduce malaria transmission level wehre it is no longer a public health problem is the goal of what is called malaria “control”. “Control” of malaria differs from “elimination” or “eradication of malaria”. “Elimination” is local or regional in scope. Eradication is “global elimination”. Eradication is not achieved until malaria is gone from the natural world. Recent increases in resources, political will and commitment have led to discussion of the possibility of malaria elimination and, ultimately, eradication. In Africa, where malaria is most common, it has been extremely difficult to control. Many reasons account for this: an efficient mosquito that transmits the infection, a high prevalence of the most deadly species of the parasite, warm climate, weak infrastructure to fight the disease, and high intervention cost that are difficult to bear in poor countries. However, the scale-up of effective, safe, and proven prevention and control interventions made possible by global support and national commitments has shown that the impact of malaria on residents of malaria-endemic countries can be dramatically reduced when these are used together.
The Global Technical Strategy for Malaria 2016–2030 (GTS) calls for reducing malaria cases and deaths by at least 40% by 2020, at least 75% by 2025 and at least 90% by 2030. Without accelerated change, these milestones will not be achieved. Insufficient levels of founding for malaria control are also a major challenge. “High burden to high impact” is a new response to the challenges of combating malaria. It consists of four key elements. First, the political will to reduce malaria deaths in highly affected countries needs to be increased. This also involves supporting grassroots initiatives that can help to create an environment of accountability and action. The second key element is to generate high-quality data and better data analysis, so that malaria control tools can be used where they are most effective. The third key element is better guidance, policies and strategies to fight malaria, which will be continually updated based on country experience and the development of new tools. And the last key element is a coordinated national malaria response, which includes not only the health sector but also environment, education and agriculture. If optimally applied, the existing package of tools for preventing, detecting and treating malaria will help to get the fight against the disease back on track and save lives. Above all, it will demand high-level political leadership, country ownership and commitment from a broad coalition of stakeholders. With more than 400 000 people projected to die this year alone from a preventable and treatable disease, we must move quickly and decisively.
References
https://apps.who.int/iris/bitstream/handle/10665/275868/WHO-CDS-GMP-2018.25-eng.pdf?ua=1
https://www.who.int/news-room/feature-stories/detail/world-malaria-report-2019
https://sustainabledevelopment.un.org/sdg3
https://www.medicalnewstoday.com/articles/150670#treatment
https://www.healthline.com/health/malaria#treatment
https://www.ecdc.europa.eu/en/malaria/prevention-and-control
https://www.cdc.gov/malaria/about/
Media Attributions
- Malaria cases in the 10 highest burden countries in Africa, 2010 – 2017