Jania Mackenthun
This article aims to elucidate on the price we pay for modernizing agriculture to feed the growing population, namely the cost to human health. I question, how can developing countries also attain the SDGs, modernizing agriculture without the detrimental impacts on human health?
Introduction
One important step in modernization is the industrialization of agriculture. Since the green revolution, humans achieved a doubling of agriculture yields to feed the growing population, though they only achieved this through a 15- to 20-fold increase in the use of pesticides (Oerke, 2006).
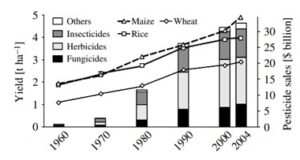
Fig. 1: World-wide yield and pesticide sales 1960-2004 (Oerke, 2006)
Still today, certain pesticides are used around the world, having dramatic acute and long-term impacts on human health. Is risking our own health the price we need to pay to feed the global population?
Human Health Impacts of Pesticides
Due to their constant exposure to pesticides, farmers and people in agricultural areas are at particular risk of acute and chronic cardiovascular and respiratory conditions (Brackbill, Cameron, Behrens, 1994). This makes them particularly vulnerable to diseases like endometriosis and some types of cancer, due to their consistent exposure to pesticides (Hoppin et al., 2006; National Institute of Environmental Health Sciences, 2022). “Innocent” bystanders of the general population, particularly those living in agricultural communities can also be exposed through inhalation, direct skin contact and ingestion. Pesticide residues can be unintentionally consumed through both raw, washed, peeled and/or cooked food and beverages (McGill & Robinson, 1968), even though they have no say in its implementation. Minute exposure impacts cardiovascular and respiratory systems, resulting in headache, skin irritation, eye irritation and fatigue, while more severe exposure can impact central nervous system, hepatic and reproductive systems. Pesticide exposure has also been linked to diabetes and obesity (Thayer, 2012).
More detailed health impacts of pesticide exposure:
- Respiratory system impacts include flu-like symptoms (Sprince, Lewis, Whitten, Reynolds, and Zwerling, 2000)
- Central nervous system reactions include parasthesias, agitation, lack of coordination, hyperaesthesia, confusion, dizziness, myoclonus and generalized seizures (with severe poisoning leading to status epilepticus and ultimately death) (Menezes et al., 2017)
- Reproductive impacts have been associated with miscarriages, particularly with thiocarbamates, carbaryl, and unclassified pesticides as well as pre-term delivery (Savitz, Arbuckle, Kaczor, and Curtis, 1997). Women living and working in agricultural communities are more likely to experience infertility concerns and males to experience infertility (Fuortes, Clark, Kirchner, & Smith, 1997; Wharton & Foliart, 1988).
- Developmental affects associated with fetuses exposed via mother include oral-facial clefts (Nurminen, 1995), limb reduction and organ system anomalies (Lin, Marshall, & Davidson, 1994). Pregnance exposure can also result in hampered brain- and behavioral development and mental health for the child (Sagiv et al., 2010).
- Endocrine disrupting pesticides bind and alter neurotransmitter binding sites, which can cause a whole host of issues, like altered estrogen production, altered testosterone levels, change androgen availability, thus disrupting reproductive and sexual development (Mnif et al., 2011)
- Dermatologically, pesticides can act as allergic or irritant dermatitis. Rare clinical forms also occur, including urticaria, erythema multiforme, ashy dermatosis, parakeratosis variegata, porphyria cutanea tarda, chloracne, skin hypopigmentation, nail and hair disorders. Exposure to arsenic pesticides can increase risk of skin cancer (Spiewak, 2001)
- Gastrointestinal effects have been present even in acute exposure, resulting in nausea, stomach cramps and diarrhea (Eaton et al., 2008). Broader change from pesticides to the gut bacteria can result in inflammatory bowel disease, obesity and diabetes (Sokol et al., 2008; Bäckhed et al., 2004; Zhao, 2013)
- Carcinogenic: Numerous cancers have been linked to pesticide exposure. Those exposed as fetuses are more likely to develop childhood leukemia and adult breast and testicular cancer (Wigle, Turner & Krewski, 2009). Positive correlations have been found in most studies between pesticides and non-Hodgkin lymphoma and leukemia (Bassil et al., 2007)
Endosulfan: a case example for continued pesticide use
Endosulfan is an interesting case example that illustrates how, despite detrimental health impacts and international bans, certain pesticides can continue to be produced and used. Endosulfan is an organochlorine insecticide similar in chemical properties, environmental fate and human health impacts as DDT, a pesticide banned in 2001 via the Stockholm Convention. Endosulfan fulfils all the hazard criteria for classification as a persistent organic pollutant under the UN-ECE (LRTAP) Protocol (UNECE, 1998) and the UNEP Stockholm Convention (UNEP, 2001). Despite international recognition of detrimental effects of organochlorines, Endosulfan was exempted from the Stockholm convention in 2004 (UNEP, 2001). It took until 2007 for it to be nominated and ultimately implemented in 2011. Endosulfan is thought to be a reason for issues with the male reproductive tract, leading to decreased sperm count, hypospadias, cryptorchidism and testicular cancer (Menezes et al., 2017). Endosulfan is has also been clearly linked to respiratory problems, such as chronic cough, phlegm production and wheezing. One study concluded that spending just 30 days per year applying endosulfan in an agricultural position leads to such symptoms (Quansah et al., 2016). Endosulfan can accumulate in pregnant women and be transferred to their fetus and has been found in human breast milk (Pirsaheb, 2015). Such exposure is associated with stinted fetal growth, immunotoxicity, cancer and metabolic, neurodevelopmental and reproductive disorders (Muller et al., 2017).
The Path Forward
In developed countries, socio-political processes have increasingly banned more pesticides over time, following convincing research like those presented above. Despite being accepted to the list of banned chemicals by the Stockholm Convention in 2007, endosulfan is still being produced and used, particularly in developing countries.
Despite its recognized flaws, Modernization Theory shows us how developing countries deserve a fair chance to develop, which could imply first going through steps that lead to environmental (and argued here, human health) degradation, before developing sound socio-political processes that would reduce the use of these harmful pesticides.
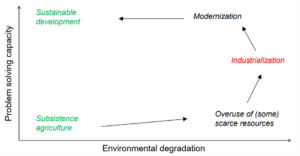
Fig. 2: Modernization perspective of development explained (Bernhauer, 2021)
This brings us back to the original question posed above: Is risking our own health the price we need to pay to feed the global population? As illustrated, technological advancement allows us to implement tools like pesticides to advance agriculture, which may be followed by environmental and health degradation; however, further problem solving capacity in society leads to scientific research and case examples of harmful effects that can in turn regulate the use of these harmful pesticides. Though a pessimistic perspective, it may imply that we need to first go through the evolution illustrated in the modernization perspective of development in order to “clean up the mess we have made.”
References
Bäckhed, F., Ding, H., Wang, T., Hooper, L.V., Koh, G.Y., Nagy A., Semenkovich, C.F., & Gordon, J.I. (2004). The gut microbiota as an environmental factor that regulates fat storage. Proc. Natl. Acad. Sci., 101(157), 18-15723. doi: 10.1073/pnas.0407076101
Bassil, K.L., Vakil, C., Sanborn, M., Cole, D.C., Kaur, J.S., & Kerr, K.J. (2007). Cancer health effects of pesticides: systematic review. Canadian family physician Medecin de famille canadien, 53(10), 1704–1711.
Bernhauer, T., (2021). International Environmental Politics: How and why do international environmental problems emerge [PowerPoint slide], Center for Comparative and International Studies, ETH Zürich.
Eaton, D.L., Daroff, R.B., Autrup, H., Bridges, J., Buffler, P., Costa, L.G., Coyle, J., McKhann, G., Mobley, W.C., & Nadel, L. (2008). Review of the toxicology of chlorpyrifos with an emphasis on human exposure and neurodevelopment. Crit. Rev. Toxicol., 38(1), 125. doi: 10.1080/10408440802272158
Fuortes, L. Clark, M.K., Kirchner, M.L., & Smith, E.M. (1997). Association between female infertility and agricultural work history. American Journal of Industrial Medicine, 31(4), 445-51.
Hoppin, J., et al. (2006). Environmental Exposure Assessment of Pesticides in Farmworker Homes. Environmental Health Perspectives, 114(6), 929-935, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1480520/
Lin, S., Marshall, E.G., & Davidson, G.K. (1994). Potential parental exposure to pesticides and limb reduction defects. Scandinavian Journal of Work and Environmental Health, 20, 166-79.
McGill, A.E., & Robinson, J. (1968). Organochlorine insecticide residues in complete prepared meals: a 12-month survey in S.E. England. Food Cosmet Toxicol, 6, 45–57. doi:10.1016/0015-6264(68)90080-1
Menezes, R.T., Qadir, T.F., Moin, A., Fatima, H., Hussain, S.A., Madadin, M. Bilal, S., Fatima, A., Rubaish, A., & Senthilkumaran, S. (2017). Endosulfan poisoning: An overview. Journal of Forensic and Legal Medicine, 51, 27-33. https://doi.org/10.1016/j.jflm.2017.07.008.
Mnif, W., Hassine, A. I., Bouaziz, A., Bartegi, A., Thomas, O., & Roig, B. (2011). Effect of endocrine disruptor pesticides: a review. International journal of environmental research and public health, 8(6), 2265–2303. https://doi.org/10.3390/ijerph8062265
Muller, M.H., Polder, A., & Brynildsrud, O.B. (2017). Organochlorine pesticides (OCPs) and polychlorinated biphenyls (PCBs) in human breast milk and associated health risks to nursing infants in Northern Tanzania. Environ Res, 154, 425-434.
National Institute of Environmental Health Sciences. (2022). Endocrine Disruptors. https://www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm
Oerke, E. (2006). Crop losses to pests. The Journal of Agricultural Science, 144(1), 31-43. doi:10.1017/S0021859605005708
Pirsaheb, M., Limoee, M., Namdari, F., & Khamutian, R. (2015). Organochlorine pesticides residue in breast milk: a systematic review. Med J Islam Repub Iran, 29, 228.
Quansah, R., Bend, J.R., Abdul-Rahaman, A. (2016). Associations between pesticide use and respiratory symptoms: a cross-sectional study in Southern Ghana. Environ Res, 150, 245-254.
Sagiv, S.K., Thurston, S.W., Bellinger, D.C., Tolbert, P.E., Altshul, L.M., & Korrick, S.A. (2010). Prenatal organochlorine exposure and behaviors associated with attention deficit hyperactivity disorder in school-aged children. Am J Epidemiol, 171(5), 593–601.
Savitz, D.A., Arbuckle, T., Kaczor, K., & Curtis, K.M. (1997). Male pesticide exposure and pregnancy outcome. American Journal of Epidemiology, 146, 1035-36.
Sokol, H., Pigneur, B., Watterlot, L., Lakhdari, O., Bermúdez-Humarán, L.G., Gratadoux, J.J., Blugeon, S., Bridonneau, C., Furet, J.P., & Corthier G. (2008). Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci, 105, 16731–16736. doi: 10.1073/pnas.0804812105
Spiewak, R. (2001). Pesticides as a cause of occupational skin diseases in farmers. Ann Agric Environ Med, 8(1), 1-5.
Sprince, N.L., Lewis, M.Q., Whitten, P.S., Reynolds, S.J., Zwerling, C. (2000). Respiratory symptoms: Associations with pesticides, silos, and animal confinement in the Iowa Farm Family Health and Hazard Surveillance Project. American Journal of Industrial Medicine, 38(4), 455-62.
Thayer, K.A. (2012). Role of Environmental Chemicals in Diabetes and Obesity: A National Toxicology Program Workshop Review. Environmental Health Perspectives, 120(6), 779-789. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3385443/
UNECE. Executive Body. (1998). The 1998 Aarhus Protocol on Persistent Organic Pollutants (POPs). https://unece.org/environment-policy/air/protocol-persistent-organic-pollutants-pops#:~:text=The%20Executive%20Body%20adopted%20the,three%20by%2Dproducts%2Fcontaminants
UNEP. Evaluation and Oversight Unit. (2001). Annual Report 2001. https://wedocs.unep.org/bitstream/handle/20.500.11822/286/UNEP_Annual_Evaluation_Report_2001.pdf?sequence=1&isAllowed=y%2C%20http
Wigle, D.T., Turner, M.C., & Krewski, D. (2009). A systematic review and meta-analysis of childhood leukemia and parental occupational pesticide exposure. Environmental Health Perspectives, 117(10), 1505–13.
Whorton, D., & Foliart, D. (1988). DBCP: eleven years later. Reproductive Toxicology, 2(3-4), 155–61.
Zhao, L. (2013). The gut microbiota and obesity: From correlation to causality. Nat. Rev. Microbiol., 11, 639–647. doi: 10.1038/nrmicro3089